Reducing Child Mortality, Door-to-Door
One of the biggest frustrations of anybody who works in development is how many people die from diseases which are cheap and easy to prevent, and routinely are in many parts of the world. The medical know how to defeat malaria, diarrhea and malnutrition has been publicly available for many years but billions of dollars and a half-century of effort have failed to prevent almost 3 million children from dying every year from these easily preventable diseases. Mortality remains especially high in rural areas of developing countries, as they are typically underserved by official health systems. What is urgently needed is an efficient, scalable, and sustainable mean of delivering existing medical solutions to those areas.

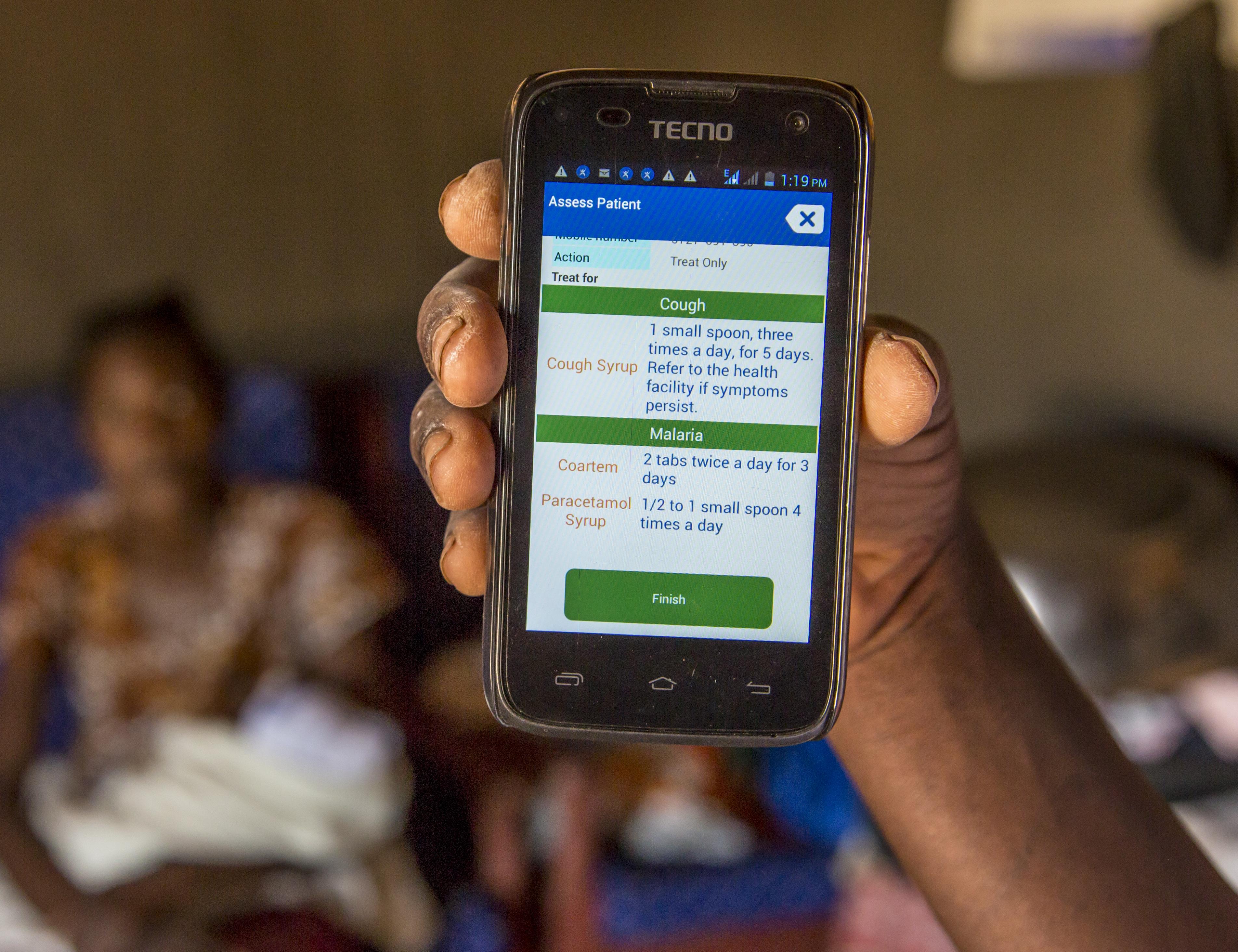
In 2007 Living Goods, a US-based NGO, in collaboration with BRAC Uganda began piloting an innovative model for solving part of the service delivery problem in rural and peri-urban areas of Uganda. The model creates “Avon-like” networks of door-to-door mobile Community Health Promoters (CHP) that provide basic health education and make a modest income by selling a diverse basket of basic health goods. The CHPs are selected through a competitive process among female village members that apply for the position in each village in which the NGOs are active. Eligible candidates receive initial training, which covers preventing, diagnosing, and treating childhood illness, recognizing danger signs for referring to a healthcare clinic, healthy pregnancy and newborn care, and nutrition. At the end of the training, a skills test is administered to determine who can become an active CHP. Selected CHPs also attended a one-day training each month to review and refresh key topics.
The main activities of the CHPs consist of conducting home visits within their own communities, educating households on essential health behaviors, providing basic medical advice, referring the more severe cases to the closest health center, and selling preventive and curative health products. The product line the CHPs have at their disposal includes prevention goods (e.g. insecticide-treated bednets, water purification tablets, and vitamins), curative treatments (e.g., oral rehydration salts, zinc, and anti-malarial drugs), and other health-related commodities (e.g. diapers, detergent, and hand soap) along with durable goods that also have health benefits (e.g. improved cook stoves, solar lights, and water filters). CHPs purchase these products directly from Living Goods or BRAC at wholesale price and earn a margin on each product sold. Thus, the CHPs operated as micro-entrepreneurs with financial incentives to meet household demand and improve child health.
A team of four researchers worked with Innovations for Poverty Action over three years to carry out a randomized evaluation of the impacts of the program. Among 214 rural villages across 10 districts of Uganda, researchers randomly assigned 115 villages to the treatment group, which received the CHP program, and 99 villages to the comparison group, which did not receive the program. The data shows that the program significantly improved households’ access to healthcare services as well as health outcomes. In particular, households of villages in the program were significantly more likely to receive the visit of a health worker, especially after having a child, or after a child fell sick with malaria or diarrhea. The program also led to improvements in health knowledge and health behavior, especially concerning the prevention and treatment of malaria and diarrhea.
Most importantly, the program reduced under-5 child mortality by 27 percent relative to the comparison group. Also infant (under-1 year) and neonatal (under-1 month) mortality significantly decreased, by 33 percent and 27 percent, respectively. The findings suggest that micro-franchise models can lead to increase access to low-cost health products and basic newborn and child health services to low-income families, leading to a significant reduction in child mortality. Based on the evidence, the program is being scaled-up. In 2013 the program was active in roughly 900 villages with a total population of 1.3 million. Within the next two years, it is estimated to reach 4.3 million individuals in more than 4,000 villages. The program is being moreover expanded to Kenya. IPA is working with the research team to evaluate whether the strong positive impacts can be sustained when the program is running at scale.
Most importantly, the program reduced under-5 child mortality by 27 percent relative to the comparison group. Also infant (under-1 year) and neonatal (under-1 month) mortality significantly decreased, by 33 percent and 27 percent, respectively.
It should be stressed that the impact of the CHP program was conditional on existing facility-based professional health care, as availability of referral services is a crucial component to the program. Thus the findings should also encourage government and non-government organizations to continue improving their facility-based care. At the same time, it also points to the importance of integrating the program into the existing health service provision strategy. We hope this evaluation's demonstration of the impact of the Living Goods model will support the ongoing collaboration between Living Goods, BRAC, and the Government of Uganda to reach as many families as possible.
Martina Björkman Nyqvist is Assistant Professor of Economics at Stockholm School of Economics. Andrea Guariso is Assistant Professor of Economics at Trinity College Dublin. Jakob Svensson is Professor of Economics at the Institute for International Economic Studies, Stockholm University. David Yanagizawa-Drott is Professor of Development and Emerging Markets at University of Zurich.












